SARS-CoV-2 (COVID-19) virus is an infectious and hence it is potentially hazardous when it comes to sample collection. There are many things which needs to be carried out with certain manner. Otherwise, it will contaminate your environment and spread the infection.
So, in this article proper sample collection of oropharyngeal and nasopharyngeal specimens separately been described in a step-by-step manner.
6 STEPS for sample collection for COVID-19 are:
- Prepare yourself with Personal protective Equipment (PPE)
- Specimen labelling and processing
- Prepare the patient
- Sample Collection Procedure
- Proper Biomedical waste disposal
- Hand Hygiene (Hand washing/rubbing)
STEP 1: Prepare yourself with Personal protective Equipment (PPE):
- Collect and handle your specimens wearing Personal protective equipment like- Apron, N95 masks, gloves, face shield etc.). All respiratory specimens need to be processed, handle with all biosafety precautions.
- Ensure PPE (eye protection, N-95 mask, long sleeved gown and gloves) while collecting and handling laboratory specimen. Use of double gloves- preferable.
- Make sure the mask fits properly.
STEP 2: Specimen labelling and processing:
Proper labelling of specimens needs to be done with appropriate details of the patients like- Name/age/gender/specimen ID, on specimen container. Details of sender like- Name/address/phone number, should be mentioned and sealed with the outer container. The outer container must be labelled with “To be tested for2019-nCoV”. These guidelines are given by ICMR-NIV, Pune (India).
STEP 3: Prepare the patient:
- Select your sample collection room to be well lighted area.
2. Place your patient in a comfortable position facing light source.
3. While collection, avoid touching anywhere of swab to prevent contamination
4. Taking out swab from protective packing.
5. Hold the swab firmly through handle.
6. DONOT touch any surface with swab after it is removed from the protective packaging.
Essential samples to be collected:
As the protective packing comes with 2 swabs (thin swab- for nasopharyngeal and thick swab for oropharyngeal) and one swab also. The important specimens for COVID-19 infection are:
1) Throat swab (oropharyngeal swab).
2) Nasal swab (Nasopharyngeal swab)
Details of Specimen collection: (Adapted from the WHO guidelines on 2019-nCoV):
| Type of Specimen | Type of swab | Transport temperature | Storage criteria | Comments |
| Nasopharyngeal/Oropharyngeal swab | Dacron or Polyester flocked swab | 4℃ | <5days (+4℃) >5days (-70℃) | Both nasopharyngeal and oropharyngeal swab is collected on same VTM to increase the viral load. |
| Broncho-alveolar Lavage | Sterile container | 4℃ | <48 hours (+4℃) >48 hours (-70℃) | Dilution of pathogen is common but worth sample to be taken. |
| Tracheal aspirate | Sterile container | 4℃ | <48 hours (+4℃) >48 hours (-70℃) | – |
| Sputum | Sterile container | 4℃ | <48 hours (+4℃) >48 hours (-70℃) | Ensure to collect sputum from lower respiratory tract. |
| Biopsy tissue | Sterile container with normal saline | 4℃ | <24 hours (+4℃) >24 hours (-70℃) | Autopsy biopsy should be avoided. |
| Serum – 2 samples (Acute and convalescent) | Serum separator tube (For adults- 3-5ml of blood) | 4℃ | <5days (+4℃) >5days (-70℃) | 2 samples: Acute: 1st week of illnessConvalescent- 2-3 weeks after the illness |
For transport, VTM (viral transport medium) with antibiotics and antifungal supplement is the best for Viral detection.
Repeated thawing and freezing are to be avoided as it hampers the quality of the specimen.
Best Time for sample collection is
From 3 days of symptom onset to not more than 7 days.
Preferably before starting of antimicrobial treatment or chemoprophylaxis.
Materials for collection of swabs:
Viral Transport Medium (3 ml sterile VTM) (Hi Viral transport medium-Hanks Balanced Salt Solution. Code: MS2760 A)
Sterile Dacron/Nylon flocked swab.
Phosphate buffer saline can be used in place VTM (In case, VTM is not available)
STEP 4: Sample Collection Procedure:
Two swabs to be taken – the nasopharyngeal and oropharyngeal swabs should be placed in the same tube to increase the viral load. If it’s not possible, one is enough.
Obtaining an Oropharyngeal/ Nasopharyngeal specimen:
Nasopharyngeal swab collection:
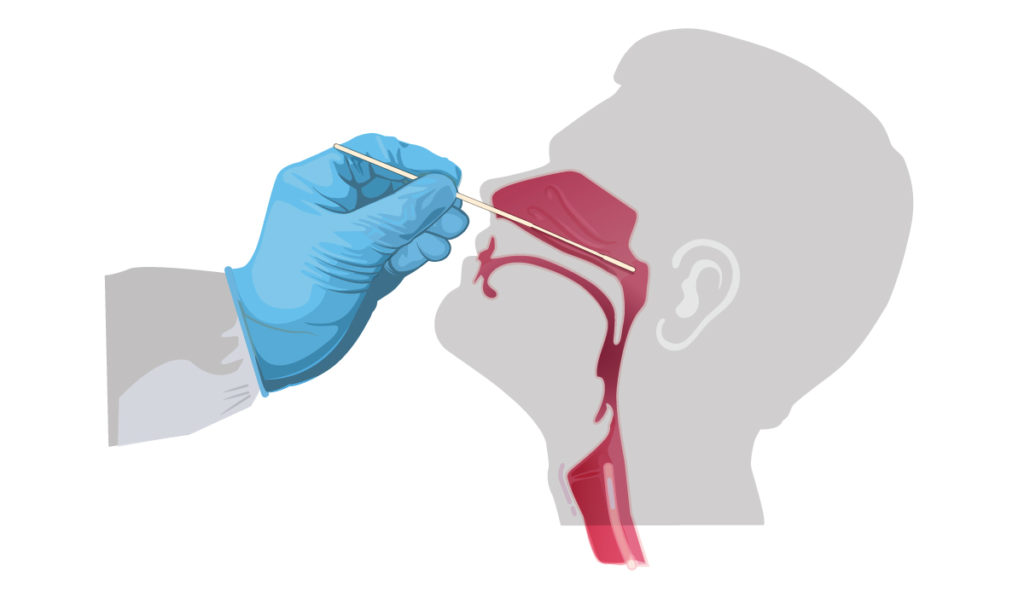
- Tilt your patient’s head back at 70 degrees
- Insert thin swab into nostril (Swab should reach depth to distance from nostrils to outer opening of the ear)
- Remain their till 5 seconds and slowly remove the swab while rotating it.
- Dip the applicator tip of swab into VTM and it is break/cut off from the mark gien in applicator stick of nasopharyngeal swab.
Oropharyngeal swab collection:
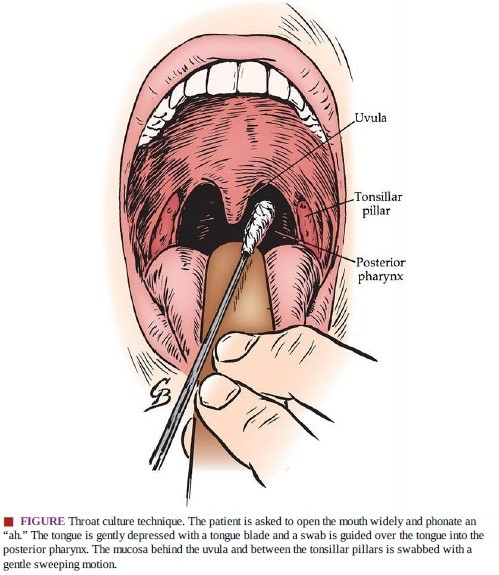
- Instruct your patient to wide open his mouth as possible he/she can.
- Instruct your patient to say “aahh”. it will elevate uvula, so that you can see full oropharyngeal area.
- Firmly hold the swab stick and take the sample with a sweeping motion to tonsillar pillars
- and posterior pharyngeal wall.
- Do not touch patients tongue or anywhere else with swab tip.
- If a “gag reflex” is seen, don’t worry it is very common and it tells you have taken a good sample.
Guidance for specimen Collection:
- Consider all received specimens as POTENTIALLY HAZARDOUS / INFECTIOUS.
- Handle all specimens in a secure manner by using gloves.
- Place each specimen into a separate container labelled with the patient’s name and identification number, the collection site, the date of collection and the time of the collection.
- Special precaution should be carried out while handling the specimen. Don’t touch the outer surface of the container with contaminated gloves.
Rejection Criteria:
- Expired transport media
- Frozen swab
- Request foe anaerobic culture
- Dry swabs
- Label not matching with that of online requisition or lab requisition form in case online requisition is not there
STEP 5: Proper Biomedical waste disposal:
Make sure the used PPE is disposed as per hospital BMW guidelines. Don’t reuse.
Biomedical waste disposal rule according to 2016 must be followed.
All infected waste should be discarded in Yellow bin.
All infected plastic wastes should be discarded in Red Bins.
All non-infected/ general waste should be discarded in Black bin.
All glass ware & metallic items discarded in blue bins.
All sharps should be discarded in white bin.
STEP 6: Hand Hygiene (Hand washing/rubbing)
Hand washing should be done according to WHO guidelines.
In case, if Hand wash facility is not available at your place, do hand rub (according to WHO guidelines) after doing sample collection procedure.